Social Safety Net Mitigates the Impact of Poverty on Brain Development and Mental Health
By David G. Weissman, Mark L. Hatzenbuehler, Mina Cikara, and Katie A. McLaughlin, Harvard University; and Deanna M. Barch, Washington University
In a recent study, we explored the relationship between state-level macrostructural characteristics, such as cost of living and anti-poverty programs, and the magnitude of socioeconomic disparities in brain development and mental health. To do so, we analyzed data covering more than 10,000 children across 17 US states. We found that lower income was associated with smaller hippocampal volume (a brain region involved in learning and memory) and higher internalizing psychopathology (denoting conditions such as depression and anxiety).
These associations were stronger in states with higher cost of living. However, socioeconomic disparities in hippocampal volume were reduced by 34 percent in high-cost-of-living states that provide more generous cash benefits for low-income families. In these states, the association of family income with hippocampal volume resembled that in states with the lowest cost of living. We also observed similar patterns for internalizing psychopathology.
Our findings suggest that generous state-level anti-poverty policies may help to address the relationship of low income with brain development and mental health, particularly in states with high cost of living.
Key Facts
- Children from low-income families are more likely to experience developmental and behavioral challenges, relative to children from high-income families.
- In states with a more generous safety net, socioeconomic disparities in hippocampal volume were 34 percent lower, with mental-health disparities similarly reduced.
- More generous anti-poverty policies may help to mitigate the developmental difficulties faced by children from low-income families, especially in states with a high cost of living.
Background
Adults raised in families with lower income as children have lower educational attainment, are more likely to rely on public assistance, and tend to have more mental and physical health problems than those raised in higher-income families.[1,2,3] Family income is associated with structural differences in the developing brain, which may contribute to disparities later in life.[4,5,6] For example, children from families with lower income are more likely to experience smaller hippocampal volume as a result of greater exposure to stressful life events. They are also more likely experience poor mental health.
However, broad social and economic factors can influence the strength of these associations between low income, mental health, and neural outcomes. For instance, living in a region with a high cost of living may enhance financial strain for families with low income and magnify the impact of low income on children’s hippocampal volume and mental health. Conversely, the generosity of the social safety net for low-income families, reflected in government programs designed to help families in poverty, may lessen that impact. However, the availability and generosity of three such programs—Medicaid, Temporary Assistance for Needy Families, the Earned Income Tax Credit— varies widely across U.S. states.
Examining Associations Between State-Level Factors and Socioeconomic Disparities
In our study,[7] we leveraged data from the Adolescent Brain and Cognitive Development (ABCD) study from 10,633 9-11-year-old youth (5115 female) across 21 sites in 17 states. These sites differed in terms of their cost of living and anti-poverty policy climates. From these data, we extracted the following measures: family income, hippocampal volume, internalizing and externalizing problems, and state-level moderators including cost of living, cash assistance, and Medicaid expansion through the Affordable Care Act. We then explored the relationships between these different measures to examine whether cost of living and the generosity of a state’s social safety net for low-income families moderated the association of family income with hippocampal volume and mental health outcomes.
Neural and Behavioral Disparities Greatest in States with Higher Cost of Living and Weaker Safety Net
We found that hippocampal volume was larger for participants with higher family income (see Figure 1). We observed a three-way interaction between family income, cost of living, and generosity of cash assistance programs in predicting hippocampal volume. Further analysis of this interaction revealed that low-income participants living in states with high cost of living and high cash benefits have hippocampal volumes that are on average 60 mm3 larger than low-income participants living in states with high cost of living and low cash benefits. More generous cash benefits at the state level are associated with income disparities in hippocampal volume that are about 34 percent lower in states with high (vs. low) cost of living. These findings suggest that cost of living and the generosity of anti-poverty policies are associated with hippocampal volume only for children in low-income families who are eligible for the benefits of these programs.
We observed a similar three-way interaction between family income, cost of living, and Medicaid expansion in relation to hippocampal volume. This revealed that, among children living in states with higher cost of living, the association between family income and hippocampal volume was weaker in states that expanded Medicaid than in states that did not.
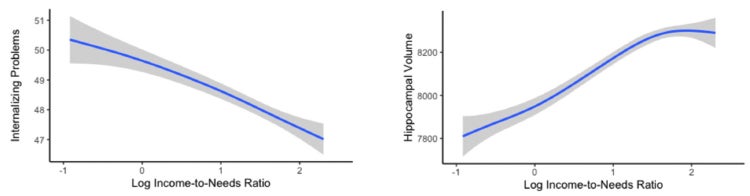
Figure 1: A higher income-to-needs ratio was associated with greater hippocampal volume and fewer internalizing problems.
We also examined whether cost of living and the generosity of anti-poverty programs moderated the association between family income and adolescent internalizing and externalizing problems. We found that, among children living in states with a higher cost of living, the association between family income and internalizing problems was lower in states with more generous anti-poverty cash assistance programs and in states that expanded Medicaid (relative to states with less generous cash assistance and that did not expand Medicaid, respectively). More generous cash benefits were associated with income disparities in internalizing symptoms that were approximately 48 percent lower in high-cost-of-living (vs. low-) states. Notably, cost of living and the generosity of anti-poverty policies were associated with lower internalizing problems only for children in low-income families eligible for these benefits, relative to children in ineligible high-income families.
Support Low-Income Families to Reduce Socioeconomic Disparities in Brain Development and Mental Health
We found that lower family income was associated with smaller hippocampal volume and poorer mental health in early adolescence. Crucially, however, the magnitude of these associations was impacted by state-level macrostructural factors such as cost of living and generosity of anti-poverty programs. These factors may amplify or reduce stressors associated with low income. Having greater financial resources may shield families from experiencing some of the chronic stressors associated with low income that can influence hippocampal development. Further, by increasing financial resources and access to healthcare, more generous anti-poverty programs could decrease the negative impact of some stressful life events on hippocampal volume and mental health.
Our findings suggest that public policies intended to increase families’ financial resources are relevant for efforts to reduce socioeconomic disparities at both neural and behavioral levels. Given the high cost of addressing the mental health, educational, and economic challenges that result from socioeconomic disparities in neurodevelopment, investments in social safety net programs could contribute to considerable long-term financial savings. This would be in addition to improving the prospects and living conditions of the many American families experiencing socioeconomic hardship.
David G. Weissman earned his PhD in psychology at UC Davis and is now a postdoctoral fellow at Harvard University.
Mark L. Hatzenbuehler is the John L. Loeb Associate Professor of the Social Sciences at Harvard University.
Mina Cikara is an associate professor of psychology at Harvard University.
Katie A. McLaughlin is a professor of psychology at Harvard University.
Deanna M. Barch is the Gregory B. Couch Professor of Psychiatry at Washington University.
References
1. Duncan, G. J., Ziol-Guest, K. M. & Kalil, A. 2010. Early-childhood poverty and adult attainment, behavior, and health. Child Dev. 81, 306–325.
2. McLaughlin, K. A. et al. 2011. Childhood socio-economic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Soc. Sci. Med. 73, 1088–1096.
3. Peverill, M. et al. 2021. Socioeconomic status and child psychopathology in the United States: A meta-analysis of population-based studies. Clin. Psychol. Rev. 83, 101933.
4. Johnson, S. B., Riis, J. L. & Noble, K. G. 2016. State of the art review: poverty and the developing brain. Pediatrics 137, e20153075.
5. Noble, K. G. et al. 2015. Family income, parental education and brain structure in children and adolescents. Nat. Neurosci. 18, 773–778.
6. Hanson, J. L. et al. 2013. Family poverty affects the rate of human infant brain growth. PLoS ONE. 8, e80954–e80954.
7. Weissman, D.G., Hatzenbuehler, M.L., Cikara, M. et al. 2023. State-level macro-economic factors moderate the association of low income with brain structure and mental health in U.S. children. Nat Commun 14, 2085. https://doi.org/10.1038/s41467-023-37778-1









